Abstract
Introduction: Diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL) are the most common types of B-cell non-Hodgkin's lymphoma (B-NHL). R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone) is the frontline treatment for primary DLBCL and FL. Pegylated liposomal doxorubicin (PLD) is the liposome formulation of doxorubicin. R-CDOP, in which PLD was used to substitute for doxorubicin, has been recommended for patients with poor cardiac function. This study was aimed to elucidate the therapy responses and cardiotoxicity with R-CDOP and R-CHOP observed in frontline treatment of patients with primary DLBCL and FL.
Methods: From January 2015 to January 2018, 77 newly diagnosed DLBCL and 25 newly diagnosed FL patients were treated with R-CDOP or R-CHOP regimen randomly. Among the 102 patients, 67 cases were treated with R-CDOP and 35 cases received R-CHOP therapy. The regimen of R-CDOP or R-CHOP consisted of Rituximab 375 mg/m2 on cycle day 0, and along with Cyclophosphamide 750 mg/m2, PLD 35 mg/ m2 or Epirubicin 70 mg/m2 (substituting for Doxorubicin), Vindesine 3.0 mg/m2 on cycle day 1 and Prednisone 100mg/d from day1 to day5 of each cycle. This regimen was implemented every 21 days approximately. After 3 cycles, tumor response were assessed and classified as complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD) according to the Cheson criteria. Cardiac function was also evaluated, including N-terminal pro B-type natriuretic peptide (NT-proBNP), left ventricular ejection fractions (LVEF) and myocardial enzymes. Patients with a therapeutic assessment of CR/PR received another 3 cycles of R-CDOP or R-CHOP regimen. Patients whose responses were evaluated for SD/PD were withdrawn from our study. After 6 cycles, tumor responses and cardiac functions were assessed again. Then the patients were followed up every three months up to 9 months or till PD. The analyses of data were performed using SAS (statistical analysis system) 9.3. Repeated measurement of variance analysis was used to determine the statistical significances of rate differences between R-CDOP group and R-CHOP group. Other statistical data analyses were performed using the two-tailed Student's t test. All differences were considered to be statistically significant when the P value was less than 0.05.
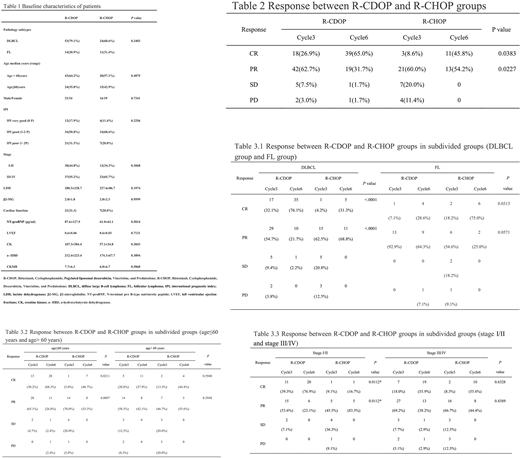
Results: The clinical characteristics were summarized in Table 1. All the patients were randomized to one of the two treatment arms. Baseline characteristics had no significant difference between the two groups. The follow up time was range from 3 to 9 months. In R-CDOP group, the CR/PR ratio was higher than that in R-CHOP group (P<0.05, Table 2). For DLBCL patients, CR/PR ratio in R-CDOP group was also higher that in R-CHOP group (P<0.05, Table 3.1). However, for FL patients, only CR ratio in R-CDOP group was higher than that in R-CHOP group (P<0.05, Table 3.1). For young patients (age≤60 years) and patients whose stage was I/II, CR/PR ratio in R-CDOP group was also higher than that in R-CHOP group (P<0.05, Table 3.2 and 3.3). However, for old patients (age> 60years) and patients whose stage was III/IV, the CR/PR ratio in R-CDOP group and R-CHOP group showed no statistical difference (Table 3.2 and 3.3).
NT-proBNP, LVEF and myocardial enzymes were measured to evaluate cardiac function. Our study showed that NT-proBNP levels had significant difference after 3 and 6 cycles treatment between R-CDOP group and R-CHOP group (62.7±44.8 pg/ml, n=29 vs. 101.0±65.0 pg/ml, n=26 and 55.6±35.6 pg/ml, n=25 vs. 103.20±57.7 pg/ml, n=25, P<0.05). Surprisingly, the difference between these two groups disappeared in follow-up period. LVEF (0.66±0.02, n=18 vs. 0.64±0.01, n=12) and myocardial enzymes, including creatine kinase (CK, 65.1±25.1 U/L, n=27 vs. 127.6±64.1 U/L, n=20) and creatine kinase isoenzyme CKMB (8.0±2.5 ng/ml, n=24 vs. 14.9±9.3 ng/ml, n=17), were found to have significant differences in R-CDOP group and R-CHOP group at 9 months after the last cycle (P<0.05).
Conclusions: Our findings in this study indicated that the R-CDOP regimen offers superior oncologic efficiency when compared to standard R-CHOP regimen in primary DLBCL and FL patients. This study also showed that the substitution of conventional doxorubicin by PLD was a safer therapeutic option for patients' cardiac function.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal